Mechanical Ventilation
Pressure Sensing Endotracheal Tube
Real time monitoring of static lung compliance
VCU researchers have developed a novel way to measure the lung pressure of patients during mechanical ventilation. Current methods for measuring true lung pressure during ventilation require the use of an inspiratory hold, which requires ventilation to be paused so that the plateau pressure of the patient can be read. This can become an extensive burden to the patient, especially if they have a critical lung condition. Additionally, current real-time pressure measurements are proximal to the mechanical ventilator and are subject to flow dependent resistance from excessive buildup of mucus. This novel device seeks to relieve these issues by incorporating a pressure sensor at the distal end of an endotracheal tube, paired with a mucus removal valve, to provide true measurements of lung compliance in real time.
The technology
This novel device consists of a modified endotracheal tube with a pressure sensor located at the distal end. Due to distal sensor location, it not subject to flow dependent airway resistance. Thus, the sensor is able to continuously report the plateau pressure and static lung compliance in real-time. This enables clinicians to more accurately monitor the health status of the lungs and determine if the lung condition is worsening or improving. Additionally, clinicians could use the readings to avoid applying high ventilator outputs which may induce barotrauma in the patient. The tube also incorporates the traditional valve leading to the balloon cuff and a mechanism which allows for the removal of mucus buildup on the sensing port, to ensure continuous monitoring.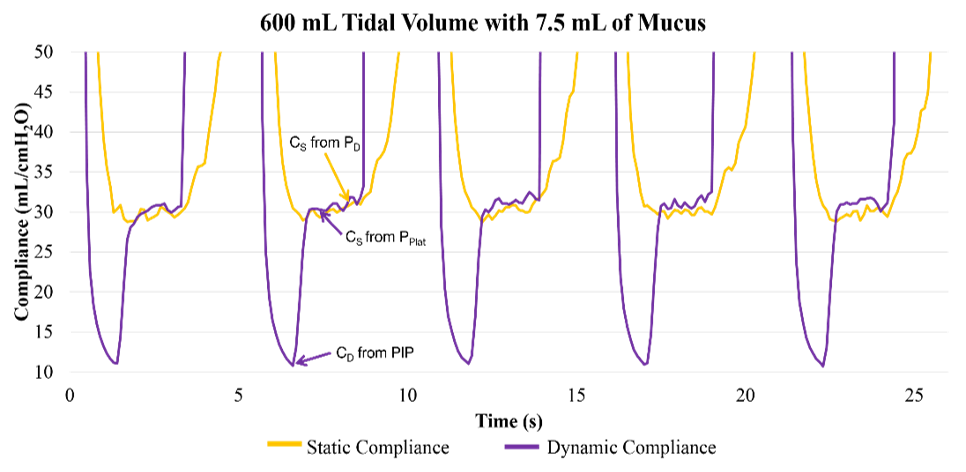
Figure 1: Graph showing real-time static lung compliance (CS - yellow) and dynamic lung compliance (CD - purple) during the 600 mL Tidal Volume with 7.5 mL of mucus trial. (PD – distal airway pressure; PPLAT – plateau pressure; PIP – peak inspiratory pressure)
